A Comparative Pilot Study Elucidating The Significance Of Low Back Dysfunction In Mobility, Balance and Lower Limb Function For Seniors And The Implications For Fall Prevention And Related Healthcare Costs
Tom J Borys MD, PhD,1 Terry W B Moore PhD (abd),1 and Albert T Oucharek HBSc.11The MMTR Neuromuscular Research Institute
The objective of this study was to compare outcomes of the unique proprietary therapy Moore MyoWorx, to an active control of conventional Physiotherapy treatment when treating seniors with non-specific low back pain. The study measured outcomes for low back pain and strength, abdominal strength, lower extremity pain and strength, balance and mobility. The purpose was to compare these outcomes between groups and to ascertain implications for related function and future care costs for seniors. This was a prospective controlled trial with single-blinded outcome evaluation held at a Senior citizens residence in Kitchener/Waterloo, Canada.
Seventeen individuals who reported lower back pain, aged 65 to 91 participated in the study. Exclusions included individuals incapable of walking, too ill to participate, and those who were terminally ill. There were eight residents included in the control physiotherapy group (AC) versus nine in the Moore MyoWorx treatment group (TX). Measurements were taken prior to the study and at one and two months into the study.
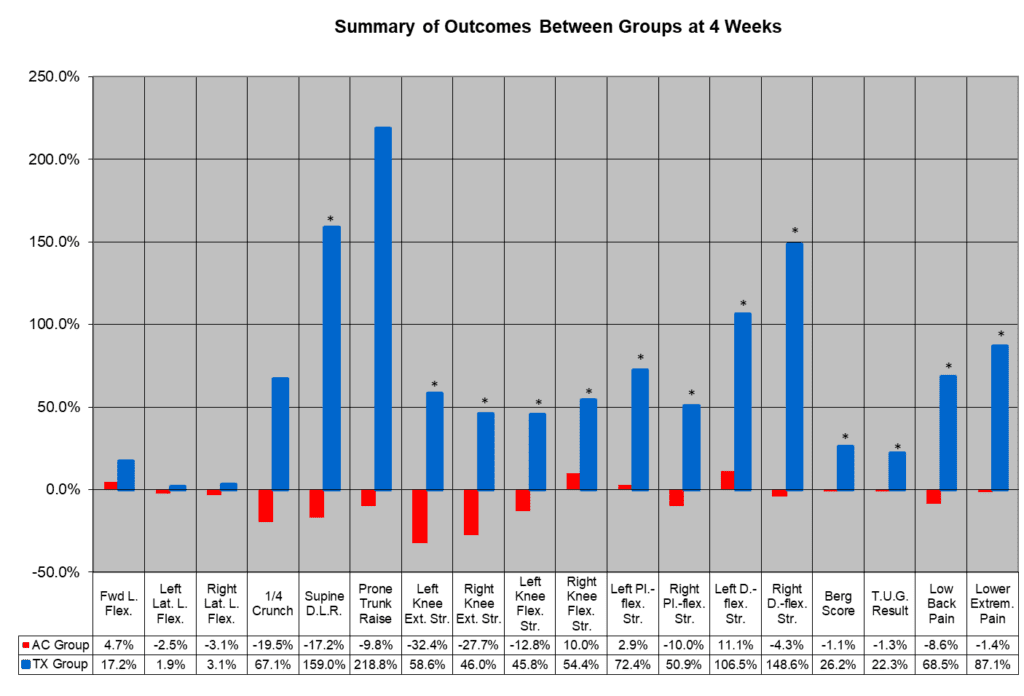
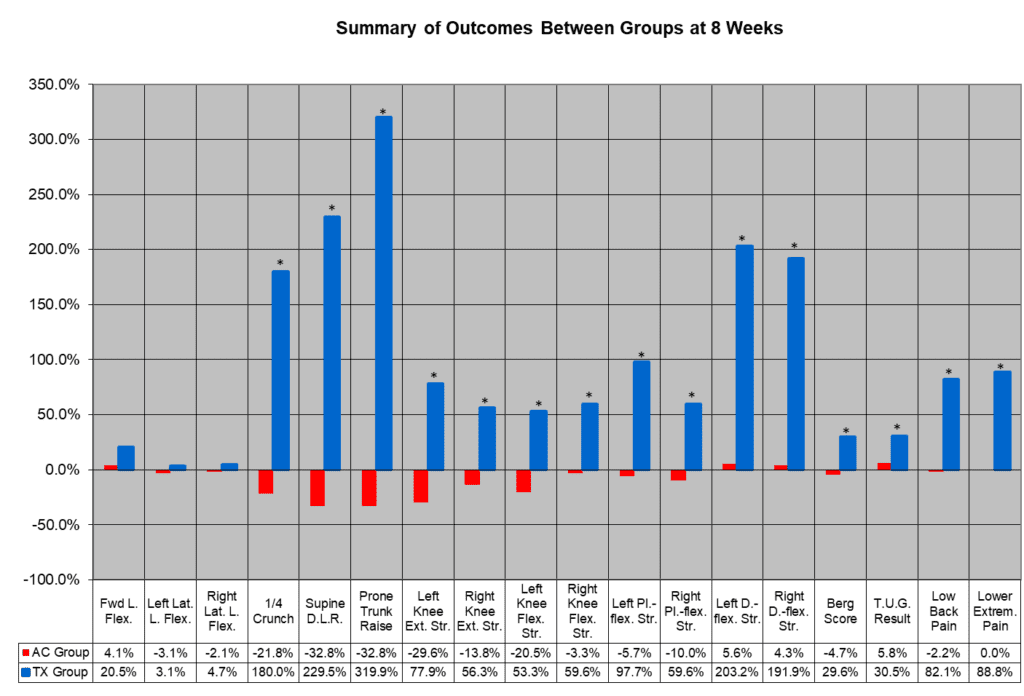
Baseline demographics and initial outcome measures were similar between the groups. Analysis of the results indicated a significant (P<.05) improvement of the Moore MyoWorx TX group versus the AC group in 9 of 13 outcome measures after one month and for 11 of 13 outcome measures after two months.
We concluded that falls and the future costs of healthcare for the aging North American population almost certainly can be reduced using the Moore MyoWorx TX group therapeutic approach, which significantly increases limb strength, mobility and balance via a low back treatment regimen and can help seniors stay active.
INTRODUCTION
Although the prevalence of low back pain in the senior population is not known with any certainty, it is estimated that 8 of 10 people experience low back pain in their lifetime.1, 2
Statistics indicate that Americans spend at least $50 billion annually in dealing with low back pain issues.3 For seniors, low back pain tends to last for longer periods and more frequently recurs, and studies have shown that elders are typically undertreated for their pain symptoms.4, 5 Other statistics indicate that those reporting low back pain are three times more likely to be in fair or poor health and four times more likely to experience serious psychological distress as compared to people without low back pain.6
When considering non-specific low back pain, one must consider what role to attribute to the muscles of the low back being weak or tight or in a degree of spasm. The low back musculature plays an integral part in providing and maintaining stability and strength to the lower spine and the ‘core’ of the body. If this ‘core’ region is dysfunctional as the result of lower back pain, then there is an associated propensity toward lower extremity injury such as with the knee joint.7 Those suffering from low back pain have also been noted to have associated leg strength deficits.8 Further support for the relationship between muscle weakness in the low back and quadriceps function has been noted and replicated in two studies by Suter, 2001 and Hart et al., 2005.9, 10
Low back pain can also adversely affect mobility and balance. Reduced mobility within the senior population often translates into long term dependence on others, or even the need to move into nursing care facilities. It is important to address mobility issues early on to improve quality of life and provide significant health benefits to this population, even quantity of life.11 Mobility and balance limitations increase the risk for falls.
In a clinical context, low back pain is typically treated as such without a realization of the further impact low back pain and low back muscle dysfunction has on other areas pertaining to safety, quality of life, and future care costs, particularly for seniors. However, evidence is gradually surfacing that suggests low back pain or dysfunction of the muscles has a significant impact on lower extremity function. A recent study indicated that subjects with chronic low back pain, as a group, demonstrated significant differences in their standing balance as compared to a healthy control group.21 With this study, we hope to elucidate that a general approach or template for treating low back pain can and should exist with the inclusion of realizing the important role that properly functioning low back muscles play in a variety of conditions, injuries or ability manifestations, which in the senior population are commonly attributed to the aging process. This could then impart a model for the treatment, but also prevention of such issues and matters.
Subjects
Eligibility for the study was open to seniors who reside in or near to a large senior’s home. Subjects were required to have the chief complaint of low back pain with or without the accompaniment of symptoms in the lower extremities and be medically cleared to participate in an active rehabilitation program. We asked for volunteers to partake in this study and there were 17 individuals who enlisted. The only selection process was that those who were referred to physiotherapy by their physician would proceed with traditional physiotherapy and the remainder would be part of the treatment group. Unfortunately, due to the small size of the study, the assessor was not blinded and hence it was a single blind study. Exclusion criteria included, severe osteoporosis, or those not deemed medically fit by the physician. The average age of subjects was 82.6 (St. Dev. +/- 7.7 years). The ages of subjects ranged between 65 to 95 years.
Intervention Groups
Subjects were divided into two groups; Active Control (AC) Group: Physiotherapy Treatment (as provided by an independent company on-site at seniors’ home) and the Treatment (TX) Group: Moore MyoWorx Treatment. The AC group had 8 subjects, average age of 83.8 (St. Dev. +/- 6.4 years), whose ages ranged between 75 to 95 years. The TX group had 9 subjects, average age of 81.6 (St. Dev +/- 8.9 years), whose ages ranged between 65 to 91 years.
Description of Interventions
Both groups worked within the following parameters: The Moore MyoWorx TX group received their intervention up to 2 times per week for 8 weeks and the AC group received the conventional intervention of Physiotherapy treatment 2 or more times per week for 8 weeks as indicated by the subjects. Both interventions were provided at separate areas located within walking distance to the subjects and fully accessible. All subjects due to advanced age had significant generalized osteoarthritis and degenerative disc disease. None exhibited signs or symptoms of disc involvement.
AC Group: Subjects who received the Physiotherapy intervention were provided the standard and conventional treatment in accordance with their chief complaint of low back pain. The intervention included use of hot packs/modalities (interferential/TENS/ultrasound) to the back and 30 minutes of active exercise for back pain and to improve or maintain mobility (core strengthening). Manual therapy techniques were also used as needed. The intervention was provided in accordance with the context of the usual service provided to the residents of the seniors’ home by an independent company.
TX Group: Subjects who received the TX intervention were provided with the prescribed Moore MyoWorx treatment in accordance with their chief complaint of low back pain. The therapeutic model consists of a proprietary process of electrotherapy known as the MyoWorx TM20. The TM20 treatment consisted of varying frequencies pulsed in a specific order and ratio of times applied to the paraspinal muscles of the lower thoracic, lumbar and sacral regions for 30 minutes; followed by 5- 10 minutes of trigger point and massage of the same paraspinal muscles; followed by 30 minutes of stretching and strengthening exercises for the paraspinal and abdominal muscles. These were the exercises given to the subjects if they were able to perform them: Sitting knee to chest, Sitting Trunk Rotation, Sitting Toe Touch, Sitting Pelvic Tilt, Lying Pelvic Tilt, Full Crunch and Prone Leg Raises.
Outcome Measures
Progress of each subject in each group was measured at the start of the study and at 1 and 2 months. There was a single assessor who measured progress for all subjects at all points who was not blinded as he also provided the TX group intervention. Though the study was to treat the chief complaint of low back pain, based on the Moore MyoWorx model for the TX group it was also important to consider the impact that treating the low back may have on lower extremity pain, strength and function regarding balance and mobility. Therefore, a total of 13 outcome measures (unilateral or bilateral) were performed from the following 7 areas of focus: Low Back Range of Motion (LBROM), Low Back Pain, Lower Extremity Pain, Trunk Strength, Upper/Lower Leg Strength, Balance, and Mobility.
Low Back Range of Motion (LBROM): Three measurements were taken for each subject to determine LBROM for forward flexion and bilateral flexion. The measurements taken were from the middle fingertip to the floor and were measured in cm.
Low Back Pain: Each subject was asked to rate their low back pain (lumbar and sacral) bilaterally using the Borg Scale. Total low back pain was tabulated by adding up the numeric scores provided for all regions of low back.
Lower Extremity Pain: Once again the subjects were asked to rate their lower extremity pain bilaterally using the Borg Scale. The subjects were asked to rate their pain in the “buttocks, hips, thighs, knees, lower legs, ankles, feet and toes bilaterally.” The total lower extremities pain was tabulated by adding up the numeric scores provided for all regions of pain noted.
Trunk Strength: Each subject was measured for their strength and endurance to perform four trunk strength tests: Quarter Crunch Position, Supine Leg Raise Position and the Prone Trunk Raise. They are instructed to hold this position as long as they are able and their capacity to do this is timed in seconds.
Strength Measurements of the Lower Extremity Muscles: Each subject’s strength was measured for knee flexion and extension, plantar-flexion and dorsi-flexion by manually using a hand held dynamometer (kg). The testing methodology followed the protocol of the “Make test”as provided in the Baseline (Registered Trademark) instruction manual for operating the Push-Pull Dynamometer.
Balance: Each subject was assessed using the Berg Balance Scale, which is an objective measure of balance abilities. It is used to identify and evaluate balance impairment in the elderly. A Berg Balance Scale score of less than 45 is predictive of multiple falls in the elderly.
Mobility: Each subject was assessed using the Timed Up and Go (T.U.G.) test. The T.U.G. test evaluates the subject’s ability to rise from a sitting position and walk a distance of 3 meters, turn around and return to a sitting position. If the subject normally uses an assistive device to ambulate then this is used during the T.U.G. test.
Statistical Analysis
Data were analyzed using Minitab version 15.0. Within group differences for all outcome measures were compared using paired t tests in cases of normal distribution of data. In cases where the distribution was not normal, within group differences were compared using Wilcoxon signed rank tests. Between group differences for all outcome measures were compared using Two Sample t tests in cases of normal distribution of data for both groups. In cases where the distribution was not normal, between group differences were compared using the Mann-Whitney U test. Significance was based upon p values 0,05.
Results
The baseline demographics and (Initial) outcome measures were similar between the 2 groups. After Month 1 (Figure 1) of the interventions, significant differences existed in 9 of 13 outcome measures between groups. These results indicated that the Moore MyoWorx TX Group demonstrated greater improvement than the AC Group in the Supine Leg Raise position, Knee Flexion and Extension strength (bilaterally), Plantar-flexion and Dorsi-flexion strength (bilaterally), the Berg Balance Scale, Timed Up and Go, Low Back Pain Ratings and Lower Extremity Pain Ratings. Lumbar Flexion and Lateral Flexion (bilaterally) were not significantly different between groups, as well as, the Quarter Crunch position and Prone Trunk Raise position.
After Month 2, (Figure 2) significant differences existed in 11 of 13 outcome measures between groups. These results showed that the Moore MyoWorx TX Group continued to have greater improvement over the AC Group in all outcome measures excluding Lumbar Flexion and Lateral Flexion (bilaterally). Also, at Month 2, 5 of 6 subjects in the Moore MyoWorx TX Group who were taking pain medications for their low back pain reported that they had stopped or decreased their dosage as compared to 1 of 6 subjects in the AC Group. As well, at Month 2, 6 of 9 subjects in the TX Group had improved in their Berg Balance Scale scores to 45 or greater (where they were <45 at Initial), compared with no subjects from the AC Group improving to 45 or greater and 1 of the 7 subjects tested having their score decrease from >45 to <45. A score of <45 on the Berg Balance scale is predictive of multiple falls.
We would like to point out that in averaged absolute values the Berg scores for the AC group were at baseline, one month and 2 months, respectively, 39.4, 39.0, and 37.6. There was a very small but consistent decline in the Berg score. Whereas for the TX group at baseline, one month and 2 months averaged absolute values for the Berg scores were respectively 35.7, 45.0, and 46.2. Although the TX group started at a lower level with the Berg score, it ended up above the designated level for increased risk of fall. Therefore, unlike the AC group, which had a decline in Berg values, the Moore MyoWorx treatment group showed improvement of 29.4%.
Discussion
Our study showed that the Moore MyoWorx TX Group provided seniors with a substantial reduction in low back pain as compared to the AC Group (conventional Physiotherapy): 82.1% for TX group versus -2.2% for AC group). This strongly supports the efficacy of the Moore MyoWorx TX group TM20 device enhancing the muscles’ ability to stretch and regain strength in the postural muscles. Additionally, our results demonstrated that the TX group therapeutic model provided seniors with a significant reduction in lower extremity pain symptoms and improvement in abdominal and back strength. It should be noted that at intake, these seniors also exhibited multiple lower leg myopathies and significant arthritic changes due to their age.
Of particular importance was the significant increase in the upper and lower leg strength, as well as the balance and mobility in the Moore MyoWorx TX group as compared with the AC group. No exercises were administered that would have the primary effect of strengthening the leg muscles. The results elucidate the importance of the paraspinal muscles not only impacting symptoms of low back pain, but also their role in effecting lower extremity pain and dysfunction. Specifically, the TX group therapeutic model suggests that tension and shortening of the paraspinal muscles may apply pressure upon the nerve roots (radiculopathies) in the lower back and hence affecting the lower extremities.7, 8, 9, 10 It is also possible that the treatment may result in a tunnel syndrome22although this is unlikely as the therapy solely affected the core muscle strength. This data significantly indicated that the loss of strength in the legs, balance, and mobility of seniors, is largely the result of lower lumbar radiculopathies. Therefore, the TX group therapeutic model depicts the need for the proprietary process of the TM20 device applied to the paraspinal muscles followed by 5-10 minutes of trigger-point massage preceding Moore MyoWorx targeted stretching and strengthening exercises, to induce effective relaxation in the muscles thereby maximizing the response of stretching and strengthening exercises and reducing the pressure on the nerve roots. It is important to note that it is physiologically impossible to strengthen a muscle that is excessively shortened or contracted and therefore one cannot strengthen the low back postural muscles. Most electrotherapies contract the muscle until the tone is reduced, and is assumed to be relaxed, whereas it is in fact fatigued and like any other muscle, will result in a rebound contraction. Thus, the results of this study not only strongly support the efficacy of the TX group therapeutic model, but also the importance to first produce effective relaxation in the muscles using the TM20 device to maximize the results of exercise. It should be noted that this treatment would not only reduce pressure upon motor neurons, but also proprioceptors in the ankles and feet, therefore, also assisting in balance.
Although it is well documented that exercises for seniors do increase their strength and mobility23, based on the data in this study, it indicates that the lower extremity muscles cannot attain their maximum strength due to neurological impingements. Hence only parts of the muscles are increasing in strength with general exercise. Therefore, this study strongly supports that a significant portion of the loss of (lower extremity) muscle strength, balance and mobility are due to radiculopathies. While general lower extremity exercise is useful in assisting seniors, it will be limited in its’ results without first addressing the radiculopathies. As a result of these previously unknown neurological deficits, we do not in fact adequately recognize the full positive effect of exercise on seniors. Based upon this study, it appears that it is possible to assist seniors with substantial musculoskeletal problems, improving function and for others, preventing significant decline. The implications of this study and its impact upon other conditions, such as cardiovascular, respiratory, “arthritic symptoms,” mental capacity decline and even type 2 diabetes, to name a few, are enormous.
For the senior population, falls can take away independence and for some, start a progression toward irreversible permanent loss of independence or even death. According to a 2005 report from the Public Health Agency of Canada, 90% of hip fractures are due to a fall and 20% of those aged 65 and older die within a year of a hip fracture.12 This creates a heavy burden on the healthcare system, where 40% of nursing home admissions are the result of falls.12 In Ontario alone, falls among those aged 55 and over accounted for $962 million in direct and indirect costs in 1999.13 Unintentional falls accounted for 59% of all emergency visits and 79% of hospitalizations due to injury. The hospitalized cases, accounted for more than 300,000 days in acute care hospitals with an average length of stay of 9.9 days. For hospitalized seniors, about 42% were discharged home (some with support services), 27% were transferred to a long-term care facility and 22% were transferred to another facility that provides inpatient hospital care.14
In the United States, more than one third of adults 65 and older fall each year.15, 16 Of those who fall, 20% to 30% suffer moderate to severe injuries that make it hard for them to get around or live independently and increase their chances of early death.17 In 2005, 15,800 people 65 and older died from injuries related to unintentional falls; about 1.8 million people 65 and older were treated in emergency departments for nonfatal injuries from falls, and more than 433,000 of these patients were hospitalized (CDC 2008). In 2000, the total direct cost of all fall injuries for people 65 and older exceeded $19 billion: $0.2 billion for fatal falls, and $19 billion for nonfatal falls.18 By 2020, the annual direct and indirect cost of fall injuries is expected to reach $54.9 billion (in 2007 dollars).19 In a study of people age 72 and older, the average health care cost of a fall injury totalled $19,440, which included hospital, nursing home, emergency room, and home health care, but not doctors’ services.20 We think it is extremely important to note that the AC group, using the conventional approach for reducing risk of fall had virtually no effect, while the Moore MyoWorx TX group improved by almost 30%, according to the Berg balance scale. At the beginning of the study, only 1 of 9 patients in the TX group were not considered to be at a high risk of fall (according to the Berg balance test) and after the study 6 of 9 patients were not considered to be at a high risk of fall. This demonstrates that not only the costs associated with falls would definitely be reduced, but that one of the reasons for seniors to require moving out of their own homes is eliminated.
It is imperative to pursue another study addressing upper body pain and dysfunction as well as the effect on proprioceptors in the neck, which also impact upon balance.
The future costs of healthcare for the aging North American population can almost certainly be dramatically reduced using the Moore MyoWorx TX group treatment and therapeutic model to increase independence, reduce care, future care costs and pharmaceutical costs.
It is imperative to conduct a larger study to further validate the therapeutic model used in the Moore MyoWorx TX group and its implications on lower extremity conditions in the senior population and how it impacts on their independence, by allowing seniors to stay in their own homes or in retirement centers, significantly deferring and in some cases, diminishing the need for nursing homes. The data strongly suggests that this approach will significantly reduce falls resulting in fractures of the bones and in particular, the pelvis. This study also strongly implies that the therapeutic model used in the Moore MyoWorx TX group is an effective means to reduce pharmacological pain management, which can lead to reduced balance and potential falls.
References
1. Acute Pain Management: Operative or Medical Procedures and Trauma. Publication No. AHCPR 92-0032. Rockville, MD: Agency for Healthcare Policy and Research, Public Health Service, U.S. Department of Health and Human Services, February 1992.
2. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. American Journal of Public Health 1992; 82(7):1020–3.
3. Bressler HB, Keyes WJ, Rochon PA et al. The Prevalence of Low Back Pain in the Elderly: A Systematic Review of the Literature. Spine: 1 September 1999 – Volume 24 – Issue 17 – p 1813
4. Cole B, Finch E, Gowland C and Nayo N. Physical Rehabilitation Outcome Measures © 1994. Published by The Canadian Physiotherapy Association)
5.Christofini Tatiana (1) ;Draibed Sergio (1) ;Sesso Ricardo (1) Evaluation of Factors Associated with Chronic Low Back Pain in Hemodialysis Patients (1) Division of Nephrology, Department of Medicine, Escola Paulista de Medicina, Federal University of Sao Paulo, Sao Paulo, Brasil The Nephron journals ISSN 1660-8151
6. Elsevier Health Sciences (2007, August 10). Better Mobility Keeps Seniors Healthier. Science Daily. Retrieved October 22, 2008, from http://www.sciencedaily.com /releases/2007/08/070809105351.htm
7. Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. Journal of Forensic Science 1996; 41(5):733–46
8. Hart et al, 2005 as cited by Hart J.M. (n.d.). Lower Extremity Consequences of “Core Dysfunction”. Virginia, United States of America.
9. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Archives of Physical Medicine and Rehabilitation 2001; 82(8):1050–6
10. Hornbrook MC, Stevens VJ, Wingfield DJ, Hollis JF, Greenlick MR, Ory MG. Preventing falls among community-dwelling older persons: results from a randomized trial. The Gerontologist 1994; 34(1):16–23.
11. Mientjes MIV, Frank JS, Neural Control Laboratory, Department of Kinesiology, University of Waterloo, Waterloo, Canada: Balance in chronic low back patients compared to healthy people under various conditions in upright standing. Presented at: The 22-Second Annual Conference of the North American Congress on Biomechanics (NACOB),
Waterloo, Ontario, Canada, 1998.
12. Mudge A, Giebel AJ, and Cutler AJ. Exercising body and mind: an integrated approach to functional independence in hospitalized older people. Journal Of The American Geriatric Society 2008; 56: 630-635
14. National Center for Health Statistics. Health, United States, 2006 With Chartbook on Trends in the Health of Americans. Hyattsville, MD: 86.
15. National Institute of Neurological Disorders and Stroke: Low Back Pain Fact sheet as accessed online at www.ninds.nih.gov.com
16. Ontario Injury Prevention Resource Centre. (2007). Injuries among Seniors in Ontario: A Descriptive Analysis of Emergency Department and Hospitalization Data. Toronto: Ontario Injury Prevention Resource Centre, 2007
17. Peri G. The critical zones of entrapment of the nerves of the lower limb. Surgical and Radiologic Anatomy1991; 13(2):139-143
18. Public Health Agency of Canada. (2005). Report on Seniors’ falls in Canada. Ottawa, ON: Public Health Agency of Canada, Division of Aging and Seniors.
19. Rizzo JA, Friedkin R, Williams CS, Nabors J, Acampora D, Tinetti ME. Health care utilization and costs in a Medicare population by fall status. Medical Care 1998; 36(8):1174–88
20. Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and nonfatal falls among older adults. Injury Prevention 2006; 12:290–5
21. Smartricks. (2006). The Economic Burden of Injury in Ontario. Toronto: SMARTRISK, 2006. In 2005-2006, seniors 65+ made 150,470 visits to Ontario emergency departments and 30,478 were hospitalized
22. Suter, 2001 as cited by Hart J.M. (n.d.). Lower Extremity Consequences of “Core Dysfunction”. Virginia, United States of America.
23. Willson J D, D. C. (2005). Core stability and its relationship to lower extremity function and injury. The Journal of the American Academy of Orthopedic Surgery, 316-325.
24. What is Neurosurgery: Low Back Pain Fact Sheet as taken from www.neurosurgerytoday.org