If you’re dealing with sciatica, you know how something as simple as sitting down can quickly turn into a painful experience. What should be a restful position often leads to sharp, shooting pain, numbness, or a deep ache that travels from your lower back down your leg. But why is sitting such a trigger for sciatic pain?
Sciatica is typically caused by compression or irritation of the sciatic nerve — the largest nerve in the body, running from the lower spine through the buttocks and down each leg. When you sit, especially with poor posture or in unsupported positions, it puts added pressure on your lower spine and the surrounding muscles. This pressure can aggravate the sciatic nerve or the tissues surrounding it, intensifying your symptoms.
Sitting for long periods also causes muscles in the hips, pelvis, and lower back to tighten and shorten. These muscles, particularly the piriformis and hamstrings, can increase tension around the sciatic nerve, further contributing to discomfort. Compounding the problem, many chairs — especially those not designed with ergonomics in mind — fail to support the natural curvature of the spine, forcing your body into awkward positions that strain nerves and muscles alike.
At Moore MyoWorx, we understand that sciatic pain is more than an inconvenience — it can disrupt your daily life and limit your mobility. The good news is that small adjustments in how you sit can make a big difference. In this post, we’ll guide you through the best sitting positions for sciatica, explain how to support your body properly, and help you understand what to avoid so you can stay comfortable — and pain-free.
How to Sit with Sciatica Without Making It Worse
Whether you’re wondering how to sit with sciatica, how to sit with lower back pain, or dealing with both, the principles are similar. When you have sciatica, sitting doesn’t have to be a painful ordeal — but it does require a bit of strategy. The key is to reduce pressure on the lower back and sciatic nerve while encouraging better alignment and support. Whether you’re at your desk, driving, or lounging at home, the goal is the same: keep your spine neutral, hips balanced, and muscles relaxed.
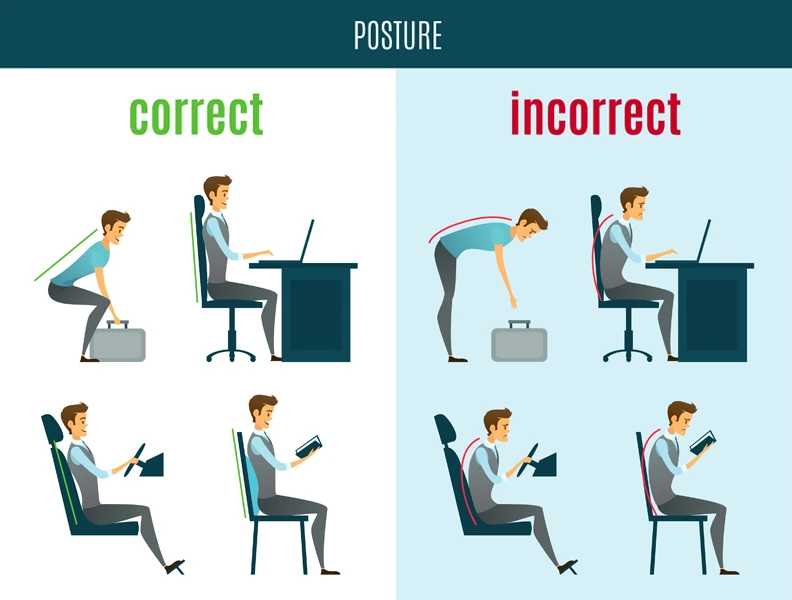
Start by choosing a seat that supports your lower back. Sit all the way back in your chair so your back is in contact with the backrest, and avoid slouching or leaning forward. Use a lumbar cushion or a rolled-up towel to maintain the natural curve in your lower spine. Your knees should be at the same height as your hips or slightly lower, and your feet should rest flat on the floor — not dangling or tucked underneath you.
If you’re working at a desk, adjust your monitor to eye level to discourage leaning forward. Take regular breaks — ideally every 30 minutes — to stand, stretch, or walk around, which helps relieve pressure and stimulates blood flow.
Driving can be particularly difficult with sciatica. Recline your seat slightly to reduce lower back pressure, and use a small cushion or lumbar support. Avoid leaning on one hip or shifting to one side for long periods.
Small, mindful changes in your sitting habits can have a big impact on managing sciatica pain. In the next sections, we’ll break down specific ergonomic strategies, how to choose the best chair, and long-term habits to prevent flare-ups — so you can sit with more comfort and confidence, no matter where you are.
Ergonomic Tips for Everyday Sitting with Sciatica
Proper ergonomics can significantly reduce sciatic pain and even prevent flare-ups altogether. The foundation of ergonomic sitting is maintaining a neutral spine — one that preserves the natural S-curve without forcing your body into unnatural positions.
Start by positioning your pelvis correctly. Sit on your “sit bones” (ischial tuberosities), not your tailbone, and avoid slouching backward or perching forward. You can use a wedge cushion or ergonomic seat pad to tilt your pelvis slightly forward, which helps keep the spine aligned and reduces pressure on the sciatic nerve.
For office or dining chairs, make sure your thighs are parallel to the floor and your feet are flat, with knees at a 90-degree angle. Use a footrest if needed. Your back should rest comfortably against the chair’s backrest, and a lumbar roll or support can help fill the natural curve of your lower back.
When it comes to sitting on a sofa — a common sciatica trap — things get tricky. Most couches are too soft and saggy, which can force you into a hunched or twisted position. If you’re wondering how to sit on a sofa with sciatica, try sitting on the edge of the cushion with your hips slightly above your knees. Add firm pillows behind your lower back and under your thighs for support. If you’re watching TV or relaxing, use a reclined position with a lumbar cushion and elevate your legs slightly to reduce tension in the lower back.
The golden rule: listen to your body. If you feel your leg or lower back starting to tighten or tingle, take it as a cue to adjust your posture or get up and move. Ergonomics isn’t a one-size-fits-all solution, but with a few smart adjustments, you can create sitting setups that work for your body and minimize sciatic irritation.
Best Chair for Sciatica: What to Look For
Choosing the best chair for sciatica can be a game-changer. A well-designed chair not only promotes better posture but also alleviates stress on the lower back and hips, preventing the sciatic nerve from becoming irritated during prolonged sitting. This is crucial for identifying the best sitting position for lower back pain and sciatica together.
First and foremost, look for adjustable features. A chair that allows you to customize the seat height, tilt, backrest angle, and lumbar support is ideal. Your hips should be slightly higher than your knees, and your feet should be flat on the floor. This encourages a forward pelvic tilt that helps maintain spinal alignment and reduces nerve pressure.
Lumbar support is critical. A chair with built-in lower back support — or one that accommodates a lumbar cushion — will help maintain the natural curve of your spine and prevent slouching, which is a major contributor to sciatic pain.
Seat depth is another important factor. You should be able to sit back fully without the seat edge digging into the backs of your knees. About 2–3 inches of space between the seat and your knees is optimal. If the seat is too deep, it may force you to slouch or perch forward — both problematic positions for sciatica sufferers.
The seat cushion should be firm but not hard. Soft, plush chairs may feel comfortable initially but often lack the support needed to prevent your pelvis from tilting backward. Memory foam or gel-infused cushions can provide a balance of comfort and structure.
Finally, if you’re sitting for extended periods — whether working from home or in an office — consider an ergonomic office chair or even a kneeling chair, which promotes upright posture and reduces spinal loading. Investing in the right chair isn’t just about comfort — it’s about long-term relief and supporting your body as it heals.
How to Prevent Sciatica Pain When Sitting
Prevention is often the best medicine, especially when it comes to sciatica. If you’re already managing symptoms or looking to avoid future flare-ups, a proactive approach to sitting is essential. It’s not just about how you sit, but how long you sit — and what you do before and after.
The first step is movement. Even the best sitting position for sciatica can become uncomfortable if held too long. Aim to stand, stretch, or walk every 30 to 60 minutes. Set a timer if needed, or build movement into your routine — take calls standing, walk while brainstorming, or stretch during breaks.
Next, strengthen and stretch. Supporting muscles — especially the core, glutes, and hips — help stabilize your spine and reduce the risk of nerve compression. Regularly stretch the hamstrings, hip flexors, and piriformis, as tightness in these areas often contributes to sciatic irritation when sitting.
Pay attention to posture outside of sitting, too. How you stand, walk, and sleep all affect spinal health. Carrying yourself with good alignment throughout the day helps relieve accumulated pressure and reduces inflammation around the nerve.
At home, be mindful of your seating choices. Swap overly soft couches for firmer chairs when possible, or modify your seating with pillows and cushions. Elevate your feet slightly when reclining, and always avoid positions that cause your spine to twist or curve awkwardly.
Finally, consider a daily self-care routine. Foam rolling, gentle mobility exercises, and proper hydration can go a long way in keeping your muscles and nerves happy. Preventing sciatic pain while sitting is a combination of smart choices, small adjustments, and consistent habits — all of which can help you feel more in control of your comfort and well-being.
Other Everyday Movements That Impact Sciatica

While sitting is one of the most common triggers for sciatica, it’s far from the only everyday activity that can aggravate the condition. Simple movements like bending, lifting, twisting, or even standing in place for too long can place strain on the lower back and surrounding muscles, potentially irritating the sciatic nerve.
Repetitive motions or poor body mechanics often contribute to muscle imbalances or tightness in the hips and lower back. For example, bending forward without engaging your core or lifting a heavy object with your back instead of your legs can put uneven pressure on your spine, increasing the risk of flare-ups. Twisting movements — like reaching behind you in the car or during chores — can compress the lower lumbar area, triggering pain that radiates down your leg.
Standing in one position, especially with poor posture or unsupported footwear, may also worsen sciatic symptoms. Muscles fatigue over time, and without dynamic movement or proper alignment, they can begin to tense and press against the sciatic nerve. Even walking can become painful if your gait is altered due to weakness or compensation.
Understanding how daily movements impact your sciatic nerve is key to avoiding unnecessary pain. The goal isn’t to avoid activity altogether — in fact, movement is vital to healing and relief — but to become more mindful of how you move and how your body responds. In the following sections, we’ll dive into specific positions and techniques you can use throughout the day — while standing, sleeping, working, or cleaning — to reduce strain on your lower back and support long-term recovery from sciatica.
Best Standing Position for Sciatica Relief
Standing might seem like a neutral position, but for individuals with sciatica, poor posture while upright can quickly lead to discomfort. The way you stand plays a crucial role in maintaining spinal alignment and minimizing pressure on the sciatic nerve.
The best standing position for sciatica starts with balance and alignment. Your feet should be shoulder-width apart, with your weight distributed evenly between them. Avoid leaning to one side, locking your knees, or shifting your weight predominantly onto one hip — all of which can throw off your posture and irritate the sciatic nerve. Keep a slight bend in your knees to avoid hyperextension and engage your core muscles gently to support your lower back.
Your spine should maintain its natural curvature. That means your pelvis shouldn’t tilt too far forward (exaggerating the lower back arch) or backward (flattening the spine). Stand tall with your shoulders relaxed and pulled slightly back, and keep your chin level rather than tilting your head forward or down.
Footwear also makes a big difference. Supportive shoes with proper arch support can reduce pressure on the lower back and improve your posture. If you’re standing for extended periods, consider using a cushioned mat and taking short breaks to walk or stretch. Shifting your weight occasionally from one foot to the other can also help prevent stiffness and reduce nerve irritation.
By standing with intention and awareness, you can avoid the postural imbalances that often worsen sciatica. Over time, this simple change can lead to noticeable improvements in your comfort and mobility throughout the day.
Best Position to Sleep with Sciatica

Getting restful sleep with sciatica can feel impossible, especially when lying down seems to intensify the pain. But the right sleeping position can make a huge difference in managing symptoms and supporting healing overnight.
The best position to sleep with sciatica depends on your body and symptoms, but most people find relief in a side-lying position. Lie on your pain-free side with your knees bent and place a pillow between your knees. This helps keep your hips aligned, reducing pressure on the lower spine and sciatic nerve. If both sides are uncomfortable, experiment with switching sides during the night.
For back sleepers, place a pillow under your knees to maintain the natural curve of your spine and relieve tension in the lower back. This elevates your legs slightly and reduces pressure on the sciatic nerve. Avoid sleeping flat on your stomach, as this can strain your lower back and neck, leading to increased discomfort.
A medium-firm mattress is often ideal for people with sciatica. It should provide enough support to maintain spinal alignment while offering enough cushioning to ease pressure points. If your mattress is too soft or too firm, consider using a mattress topper or adjusting with extra pillows.
Pay attention to your pillow height as well — your neck and head should be aligned with your spine, not tilted up or down. Good sleep posture helps reduce nerve compression and allows the muscles in your back and hips to relax.
Quality rest is essential for recovery, and optimizing your sleep position can be one of the most impactful ways to support sciatica relief long-term.
Sitting and Standing at Work: Managing Lower Back Pain
If you work a desk job or spend long hours on your feet, managing sciatica at work can be challenging. But with some simple adjustments, you can ease the strain on your lower back and create a more supportive routine.
For those who sit most of the day, your chair should promote good posture. Use a chair with lumbar support, or add a small cushion behind your lower back to maintain the natural curve of your spine. Sit with your feet flat on the ground, knees at hip level, and avoid crossing your legs, which can tilt the pelvis and irritate the sciatic nerve.
If you use a standing desk or are required to stand for extended periods, be mindful of posture and balance. Alternate your stance periodically, shift your weight gently, and try resting one foot on a small footrest or box to reduce lumbar pressure. Anti-fatigue mats can also help reduce strain on your feet and lower back.
Incorporate movement throughout your workday. Set a timer to remind yourself to stand, stretch, or walk for a few minutes every 30 to 60 minutes. Simple stretches for the hamstrings, hip flexors, and glutes can prevent muscle tension from building up.
Consider ergonomic accessories, such as a sit-stand desk, supportive footwear, or a footrest. These tools help you maintain optimal body mechanics and reduce the cumulative stress that can trigger sciatica pain.
By adjusting how you sit and stand at work, you can break the cycle of discomfort and make your workspace a place that supports — rather than aggravates — your recovery.
Doing Housework Without Straining Your Lower Back
Housework can be surprisingly taxing on your lower back, especially when you have sciatica. Tasks like vacuuming, laundry, and dishwashing often involve repetitive bending, twisting, or lifting — all movements that can aggravate the sciatic nerve if done without proper technique.
The key to pain-free housework is body mechanics. When lifting items, always bend at your knees, not your waist, and keep the object close to your body. Avoid twisting while holding something heavy — instead, pivot your feet to turn your entire body. Engaging your core as you lift or bend can also protect your lower back and reduce strain on the sciatic nerve.
For chores that require reaching or bending, such as scrubbing floors or dusting low shelves, try kneeling or using tools with extended handles. This keeps your spine in a more neutral position and minimizes the risk of overstretching your back. When doing dishes or prepping food, stand close to the counter with one foot slightly forward — this stance helps maintain better spinal alignment.
Break up tasks into smaller chunks and pace yourself. Extended cleaning sessions can cause muscle fatigue, which may worsen sciatic symptoms. Take short breaks to stretch, walk, or lie down briefly to relieve pressure on your lower back.
Footwear matters here too — wear supportive, cushioned shoes during household tasks to reduce impact and help with posture.
With a few adjustments to how you approach housework, you can stay active and productive without setting off a flare-up. Smart movement and a little planning go a long way toward protecting your back while keeping your home in order.
Positions to Avoid With Sciatica: What Makes It Worse?

When managing sciatica, knowing what not to do is just as important as knowing the right moves. Certain positions and movements can significantly increase irritation around the sciatic nerve, leading to flare-ups and prolonged discomfort. So, what are the worst moves for sciatica, and what positions should you avoid?
One of the biggest culprits is prolonged sitting — especially in a slouched or hunched posture. Sitting on soft surfaces like deep couches or recliners that don’t support the spine can cause the lower back to round, placing pressure directly on the sciatic nerve. Crossed legs or leaning to one side can also create imbalances in the pelvis and spine, aggravating symptoms.
Another common trigger is bending forward at the waist, especially without engaging your core. This movement can compress the discs in your lower back and increase nerve impingement. Similarly, twisting the spine (like when getting out of bed or turning abruptly in a chair) can irritate the nerve roots.
Sleeping in the wrong position — like on your stomach or without proper pillow support — can also strain your lower back and hips, setting off pain first thing in the morning.
If you’re experiencing sciatica, avoid positions that round the spine, compress the lower back, or keep your hips and pelvis uneven. These are classic positions to avoid with sciatica and piriformis syndrome. The key is to maintain neutral spine alignment as much as possible, whether you’re sitting, sleeping, or moving.
Is it better to rest or keep moving with sciatica?
While it may be tempting to rest and avoid movement when sciatica flares up, prolonged inactivity can actually make symptoms worse. Extended rest can lead to muscle stiffness, reduced circulation, and weakened core and gluteal muscles — all of which play a crucial role in supporting the spine and relieving pressure on the sciatic nerve.
Gentle, controlled movement is often more beneficial than staying still. Activities like walking, light stretching, and targeted exercises help reduce inflammation, improve mobility, and promote healing. Movement encourages blood flow, which delivers nutrients to affected tissues and helps flush out irritants that may be contributing to nerve pain.
However, it’s important to strike a balance. Overexertion or doing high-impact activities can also aggravate sciatica. The goal is to keep moving without pushing into pain. Avoid heavy lifting, high-intensity workouts, or sudden twisting and bending motions during a flare-up. Instead, opt for low-impact movement like swimming, yoga (with modifications), or guided physical therapy routines.
If sitting is unavoidable — such as during work or travel — make sure to change positions frequently, stand up and stretch every 30–60 minutes, and use ergonomic supports to maintain good posture. Listen to your body: if a position or movement causes more pain, stop and adjust.
In summary, while rest has its place during severe pain, staying gently active is typically the better path toward long-term relief and recovery from sciatica.
Additional Recommendations to Relieve Sciatica Symptoms

While finding the best sitting position is key to managing sciatica, there are several other strategies you can use to ease pain and support recovery. These methods are simple, often home-based, and can make a noticeable difference in how you feel day to day.
One effective approach is alternating between cold and warm compresses. Applying a cold pack to the lower back or buttock area during the first 48 hours of a flare-up can help reduce inflammation and numb the sharp pain caused by nerve irritation. After that initial period, switching to heat therapy — such as a warm compress, heating pad, or warm bath — can relax tight muscles and improve blood flow, which helps the healing process.
Gentle movement is also important. While bed rest might seem tempting, prolonged inactivity can make symptoms worse. Short walks, light stretching, or low-impact activities like swimming or using a stationary bike can help maintain mobility and reduce pressure on the sciatic nerve.
Incorporating proper posture habits throughout your day — especially when sitting, standing, or sleeping — can prevent aggravation. Make sure your spine is aligned and supported. When sleeping, try placing a pillow between your knees (side sleepers) or under your knees (back sleepers) to maintain a neutral spine.
You can also explore foam rolling or self-massage techniques to release tight muscles around the lower back and hips. Working with a specialist, like those at Moore MyoWorx, can provide a more tailored approach to long-term recovery.
Finally, stay consistent. Relief from sciatica rarely comes from a single fix, but rather a combination of habits that reduce irritation, improve mobility, and support nerve health over time.
What Is the One Movement for Instant Sciatica Pain Relief?

While no single movement works for everyone, one of the most commonly effective movements for instant sciatica pain relief is the standing lumbar extension. This simple, targeted exercise helps create space around the compressed nerve root and can reduce pressure on the sciatic nerve.
To perform a standing lumbar extension:
- Stand upright with your feet shoulder-width apart.
- Place your hands on your lower back, fingers pointing downward.
- Gently arch your back by pushing your hips slightly forward while leaning your upper body backward.
- Hold this position for 5–10 seconds, then return to neutral.
- Repeat this movement 5–10 times, depending on your comfort level.
This movement works by reversing the flexed posture we often assume while sitting, especially for long periods. When you sit, your lumbar spine rounds forward, which can cause discs or muscles to compress the sciatic nerve. The lumbar extension counters that by encouraging spinal decompression and opening up the lumbar space.
It’s important to note that this movement should feel relieving — not painful. If you experience increased pain, numbness, or tingling during or after the movement, stop and consult a professional.
Always pair this movement with good posture habits and avoid prolonged sitting in poor positions. When used correctly and consistently, this movement can offer noticeable, often immediate relief from sciatic pain, making it a go-to technique during flare-ups or when transitioning from sitting to standing.
What Is the Miracle Stretch for Sciatica?

While “miracle” might be a strong word, the piriformis stretch is often considered one of the most effective stretches for relieving sciatica pain, especially if the sciatic nerve is being irritated by tight gluteal or hip muscles.
The piriformis muscle sits deep in the buttock region, right near — and in some cases, over — the sciatic nerve. When it becomes tight or inflamed, it can compress the nerve, a condition known as piriformis syndrome. Knowing how to sit with piriformis syndrome — using cushions and hip-level alignment — can also prevent this compression. Stretching this muscle helps release pressure on the nerve and reduce referred pain.
Here’s how to do a basic seated piriformis stretch:
- Sit upright in a sturdy chair.
- Place your right ankle on your left knee, forming a figure-four shape.
- Keep your back straight and gently lean forward from the hips until you feel a stretch in your right glute and hip.
- Hold for 20–30 seconds, breathing deeply.
- Switch sides and repeat.
You can also perform this stretch lying on your back:
- Lie flat with knees bent and feet on the floor.
- Cross your right ankle over your left knee.
- Grasp the back of your left thigh and gently pull your legs toward your chest.
- Hold for 20–30 seconds, then switch.
This stretch can provide relief almost immediately by loosening up the muscle groups that tend to clamp down on the sciatic nerve. Incorporating it into your daily routine — especially after periods of sitting — can help keep symptoms at bay.
As always, avoid bouncing or forcing the stretch. Ease into it, and if you feel any sharp or worsening pain, stop and seek guidance from a specialist.
Does Elevating Legs Help Sciatica?

Yes — elevating your legs can help reduce sciatica symptoms, especially if your pain is caused by spinal compression or inflammation. Elevating the legs reduces pressure on the lumbar spine and can relieve tension on the sciatic nerve, promoting circulation and easing discomfort.
When you elevate your legs properly, it helps to flatten the lower back against the surface you’re lying on, which can decompress the nerve roots exiting the spine. This position is particularly effective during flare-ups or when resting for extended periods.
One of the best ways to elevate your legs for sciatica relief is the 90-90 position:
- Lie on your back on a firm, comfortable surface.
- Place your calves on a chair, ottoman, or a stack of pillows so that your hips and knees are both at 90-degree angles.
- Relax your arms at your sides and breathe deeply.
- Stay in this position for 10–20 minutes.
This posture encourages spinal alignment and reduces pressure on both the discs and the sciatic nerve. It’s also great to do before bed, after long periods of sitting, or whenever your symptoms feel heightened.
If lying on your back isn’t comfortable, using a wedge pillow to support your legs at an angle can provide similar relief while you sleep or rest.
That said, leg elevation is a temporary solution. It’s most effective when used alongside stretching, posture correction, and active recovery techniques. Avoid staying in any single position for too long, and always listen to your body. If elevating your legs increases pain or discomfort, adjust your setup or consult a healthcare professional for a more customized approach.
Conclusion: Small Postural Changes, Big Relief
Living with sciatica can be frustrating, especially when something as routine as sitting becomes a source of pain. But the good news is that relief doesn’t always require major interventions — sometimes, it’s the smallest adjustments that make the biggest impact. By becoming more aware of how you sit, move, and care for your body throughout the day, you can significantly reduce the intensity and frequency of sciatic pain. Even minor changes in sitting position can be your best way to sit with sciatica.
Proper sitting posture — with your spine aligned, feet flat on the floor, and hips slightly higher than your knees — can relieve pressure on the sciatic nerve and help prevent flare-ups. Supportive chairs, lumbar cushions, and frequent position changes can all play a role in protecting your lower back and keeping symptoms at bay. Pair this with intentional breaks to stretch or walk, and you create a more nerve-friendly environment for your body.
Beyond posture, small self-care strategies — like alternating cold and warm compresses, trying targeted movements and stretches, or elevating your legs during rest — can bring quick and lasting relief. These techniques help reduce inflammation, release muscle tension, and support better circulation, all of which contribute to less sciatic nerve irritation.
At Moore MyoWorx, we believe in empowering you with practical, science-based solutions to manage pain and restore comfort in your daily life. Whether you’re working at a desk, driving, or relaxing at home, the way you sit and care for your body matters. By taking a proactive approach and making mindful adjustments, you can take control of your sciatica — one small change at a time.
Remember: consistent, thoughtful action is the key. With the right strategies, even the simple act of sitting can become comfortable again. You don’t have to live in pain — relief is possible, and it starts with how you sit.